Individual Assessment & Group Learning
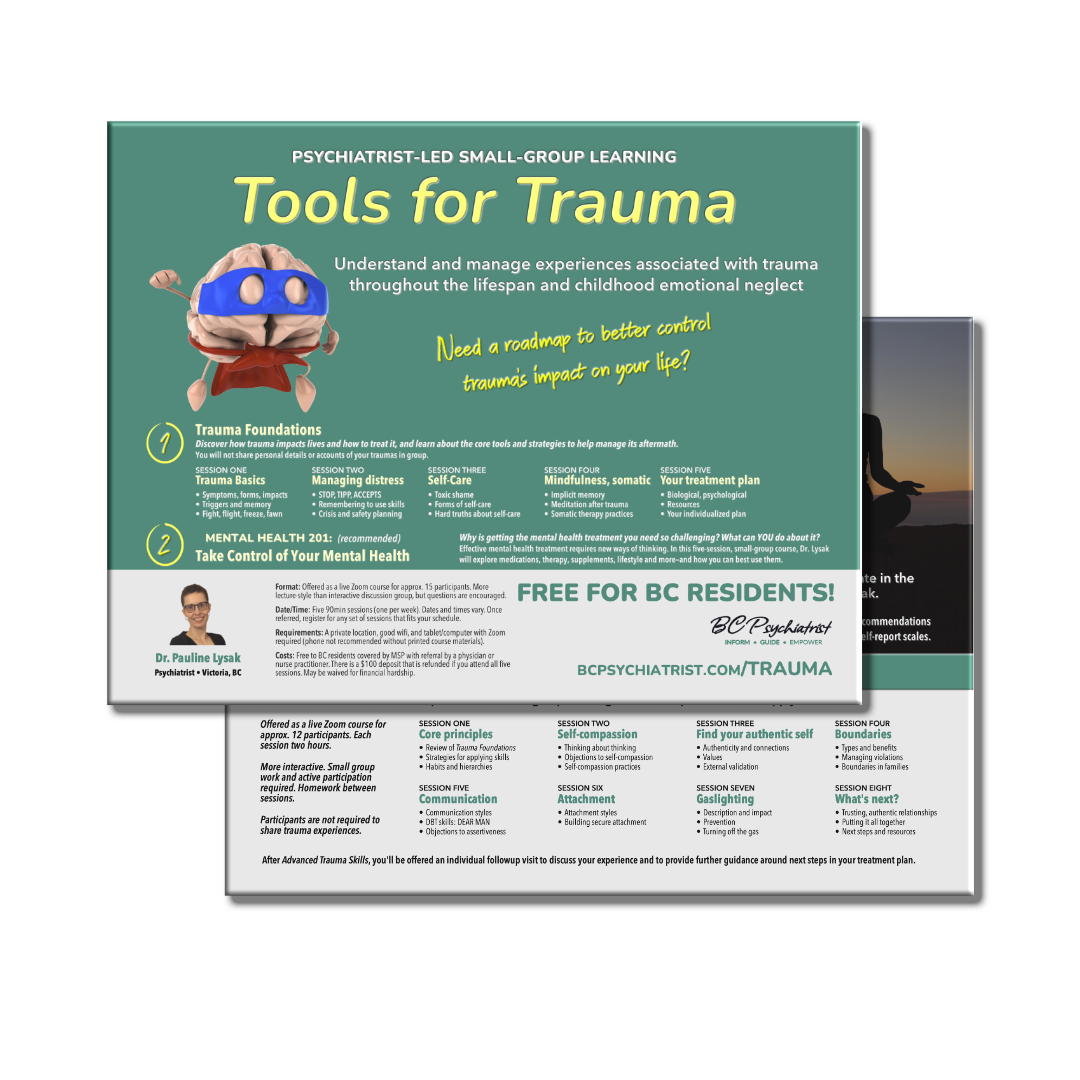
Tools for Trauma
Need a roadmap to reduce trauma's impact on your life?
Fill your toolbox with a wide range of practical tools and strategies aimed at understanding and managing the challenges following trauma throughout the lifespan and childhood emotional neglect.
Core: Trauma Foundations Education and Skills Group • Mental Health 201
Limited Capacity: Psychiatric Consultation • Advanced Trauma Skills Group
free for bc residents!
Enroll NowDownload PDF Brochure →

Trauma frequently affects mental health
Trauma comes in many forms. Violence. Abuse. Neglect. Gaslighting. Illness and its treatments. After effects can look like full-blown post-traumatic stress disorder (PTSD) or take much subtler forms.
Not all mental illness is related to trauma. But trauma can be a factor. And trauma can impair the ability to benefit from treatments commonly used for other mental illnesses.
Patients with a history of trauma are often given multiple diagnoses—depression, anxiety, panic, borderline personality—and then labelled treatment-refractory when they don't improve. The trauma component of their illness has been ignored.

Introducing
Tools for Trauma
A comprehensive program combining individual assessment and group learning
Core Program
Trauma Foundations Group
Five weekly 90min sessions via Zoom to discover how trauma impacts you and introduce you to a variety of practical tools and strategies to help manage it. You WILL NOT share personal details or accounts of your traumas in group.
Mental Health 201
(Optional) A five-week Zoom group discussing how mental health treatments work, making the most of them, and finding what's right for you. You will learn to better navigate the system and take a more active role in your care. Also available separately.
Beyond the Basics
Capacity is very limited.
Individual Psychiatric Consultation
After completing a detailed intake, you'll have a comprehensive, one-time visit to assess your overall mental health (including but not limited to trauma) and/or review your trauma history, provide treatment recommendations to you and your primary care provider.
Advanced Trauma Skills
Eight weekly two-hour sessions via Zoom that picks up where Trauma Foundations left off. Covering more advanced topics, with a focus on successfully applying skills. More interactive including small group work. You do need to actively participate in discussions, ask questions, and practice applying tools.
This program is designed for patients who are well enough to benefit from group learning, are ready, willing, and able to make changes in their own lives. People who are looking for help finding their next steps.
Trauma Foundations Group
Session One
Trauma Basics
- Symptoms, forms, impacts
- Triggers and memory
- Fight, flight, freeze, fawn
Session Two
Managing distress
- STOP, TIPP, ACCEPTS
- Remembering to use skills
- Crisis and safety planning
Session Three
Self-care
- Toxic shame
- Forms of self-care
- Hard truths about self-care
Session Four
Mindfulness, Somatic
- Implicit memory
- Meditation after trauma
- Somatic therapy practices
Session Five
Your treatment plan
- Biological, psychological
- Resources
- Your individualized plan
Mental Health 201: Take Control of Your Mental Health
Session One
Challenges and opportunities
- Health system expectations
- No silver bullet
- Trial and error, evaluation
- Diet, exercise, sleep,…
- How to influence your care
Session Two
Physical health impacts, treatments
- Physical ⇔ mental health
- Essential lab tests
- Supplements
- Medications: roles, types
- Wrong med? Here’s why…
Session Three
Antidepressants and other medications
- How they help, why used
- Starting, stopping, longterm
- Common mistakes
- Managing side effects
- Other medication classes
Session Four
Psychotherapy and novel treatments
- Types of therapy
- Providers, cost, alternatives
- Using therapy effectively
- Set goals, track results
- Psychedelics, ketamine, …
Session FIVE
Managing your care and communication
- Navigating the system
- Paging Dr. Google
- Your living treatment plan
- Evaluating treatments
- Health communication
Advanced Trauma Skills Group
Not everyone will be eligible to participate. Requires completing Trauma Foundations and Individual psychiatric consultation.
Session One
Core principles
- Review of Trauma Foundations
- Strategies for applying skills
- Habits and hierarchies
Session TWO
Self-compassion
- Thinking about thinking
- Objections to self-compassion
- Self-compassion practices
Session THREE
Find your authentic self
- Authenticity and connections
- Values
- External validation
Session Four
Boundaries
- Types and benefits
- Managing violations
- Boundaries in families
Session Five
Communication
- Communication styles
- DBT skills: DEAR MAN
- Objections to assertiveness
Session Six
Attachment
- Attachment styles
- Building secure attachment
Session Seven
Gaslighting
- Description and impact
- Prevention
- Turning off the gas
Session Eight
What's next?
- Trusting, authentic relationships
- Putting it all together
- Next steps and resources
Individual Consultation
Psychiatry Assessment, Treatment Recommendations
After Trauma Foundations, select patients may be eligible for a one-time psychiatric consultation with Dr. Lysak, and (if appropriate) then be able to participate in Advanced Trauma Skills.
This is a general mental health assessment (including but not limited to trauma) to review your history and concerns. She will provide a diagnosis, and offer individualized treatment recommendations, including medications, therapy, physical health interventions, bibliotherapy, and more.
The consultation happens during a single 90-min visit, either in-person (downtown Victoria) or via Zoom. Following the consultation, a detailed report will be sent to the primary care provider who referred you with treatment recommendations they can implement.
If you attend the Advanced Trauma Skills group, you'll be offered an individual followup visit after the group to discuss your experience and to provide further guidance around next steps in your treatment plan.
Dr. Lysak cannot provide individual treatment or ongoing care.
To make this visit as valuable as possible, she needs information from you ahead of time. You will complete a detailed intake/history form and several mental health self-report scales.
These will be reviewed, along with previous medical records (with your consent) prior to seeing Dr. Lysak.
Instead of a full consultation, patients currently followed by a psychiatrist or recently assessed by psychiatry may have a more abbreviated session, focusing primarily on their trauma history.
This is for you if:
- You know trauma holds you back, but you're not sure what to do about it, are stuck, or haven't been able to get the help you need.
- You're eager to better understand how trauma impacts you and learn tools to better manage it and improve your quality of life.
- You're willing to take on a more active role in your own care to enhance and complement what health professionals can provide.
This isn't for you if:
- You want someone else to "fix" you without any effort on your part.
- You're too easily overwhelmed, or not able to focus, learn, and participate in two-hour online sessions, or can't obtain, borrow, or use the technology to do so.
- You've got extremely specific ideas of what your care should look like and aren't open to hearing and considering other possibilities.
Ready to take the next step in your trauma journey?

What You Need to Know:
The costs of this program, including both the individual consultation and the group sessions, are covered by government health insurance (MSP).
For MSP to pay, you must be referred by a primary care provider (e.g., family doctor, nurse practitioner).
This provider can be your own doctor or NP. You can also be referred by any walk-in clinic, Urgent and Primary Care Clinic (UPCC), or online telehealth service (e.g., Telus Health).
Get referredEligibility
Open to residents of BC with MSP coverage that are significantly impacted by trauma or childhood emotional neglect (formal PTSD diagnosis not required).
Group Format
Offered as a live online course via Zoom (camera MUST be on). One session per week, each lasting 90min. Approx. 15 participants per group.
Privacy
You will not need to share accounts of your traumas in group. Identity of participants and any information voluntarily disclosed is confidential.
Costs
Covered by MSP. Groups have a $100 deposit (due when you register for particular dates) that is refunded if you attend a minimum number of sessions.
FAQ: referral and consultation
Why do I need a referral?
Can people outside BC participate?
Why is there a deposit?
Can I do the group without the consultation?
Can I do the consultation but not the group?
What if I don't like groups?
What if I don't have a primary care provider?
What if I'm triggered and in crisis?
FAQ: trauma education and skills group
Are the groups available in-person?
Can I just listen and not talk?
Can I keep my camera off?
Can I just use my phone?
What days and times is it offered?
Do I need to attend all sessions?
Get Started Today
Just follow the three easy steps below to participate in the Tools for Trauma program.
① Step One
Download the referral form to give to a primary care provider to fill out.
Or share the link to this page:
bcpsychiatrist.com/trauma
② Step Two
Ask a primary care provider to refer you to this program. They need to fill out the form you downloaded and fax it to us.
We encourage them to send additional documentation (physical and mental health history, labs, etc.) as they would for any psychiatry referral.
③ Step Three
After we get the referral, we'll be in touch with you via email within two weeks.
We'll provide you information on upcoming sessions of Trauma Foundations and Mental Health 201, as well as how to register once you find sessions that work for your schedule.
Email [email protected] if you don't hear from us within two weeks of the referral being sent.
Any Family Doctor or Nurse Practitioner can refer you.
This can be your own doctor or NP if you have one, but also any walk-in clinic, Urgent and Primary Care Centre (UPCC), or online telehealth service (e.g., Telus Health).